You may have seen the recent coverage regarding patients receiving a co-payment bill from a follow-up colonoscopy to a positive Cologuard test. If you haven’t, below are several links to the story in various media. CBS News: Woman hit with nearly $2,000 unexpected bill for colon cancer screening U.S. News & World Report: Could Home Test for Colon Cancer Mean a Big Medical Bill to Come? People: Missouri Woman Billed $1,900 for Colonoscopy After Previously Taking an At-Home Cancer Test One issue not mentioned in the article is that many of these test results could be false-positive, leading people to worry about having polyps or cancer and facing a potential co-payment even though the colonoscopy is negative. A recent study of 450 patients presented at Digestive Disease Week in May 2021 found that only two percent (2%) of patients with a positive stool test had colon cancer. And, two-thirds of the patients tested had a false-positive result, which may have resulted in more out-of-pocket expenses for a diagnostic colonoscopy to validate the findings of the home test, as described by the news reports. Alternatively, most insurance providers would cover a simple colonoscopy screening that detects and prevents colorectal cancer as a preventative measure. Colon cancer claims over 50,000 lives every year and is the 2nd most common cause of cancer death in the U.S. Colon cancer is preventable, treatable, and beatable – but only with early and accurate detection. Because colon cancer often begins as growths in the colon called polyps, finding and removing polyps is the best way to prevent colon cancer. There are three types of colorectal cancer (CRC) screening:
- Colonoscopy – 95% of large polyps detected
- Stool DNA (Cologuard) – 42% of large polyps detected
- Fecal Immunochemical Test (FIT) – 30% of large polyps detected
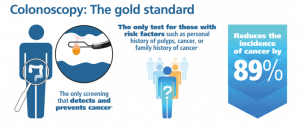
Potential polyps identified through a positive FIT or a Cologuard test require a colonoscopy to remove the polyps. Unfortunately, large polyps can go undetected with FIT and Cologuard tests. When polyps aren’t found and removed, it increases the risk of developing colon cancer. Colonoscopy remains the gold standard for finding polyps. Polyps found during a colonoscopy are removed during the procedure, eliminating the need for additional procedures. The U.S. Preventative Task Force (USPTF) recently recommended that colorectal cancer screenings start at age 45 vs. 50. As a result, an additional 22M people age 45-49 need to be screened for colon cancer this year alone. Although home screening kits may seem like a more accessible, more cost-effective means, the fact remains that a colonoscopy is the only screening method that can detect and prevent colon cancer.
Colon Cancer Detection vs. Prevention
Cologuard is designed only to detect cancerous indicators (DNA) in the fecal sample provided. However, 58% of the time, dangerous precancerous polyps are not detected at all with Cologuard. A Cologuard test is considered a screening test and requires repeating every three (3) years if initial test results are negative. Cologuard is known to provide a significant percentage of False Negative and False Positive results. In a recent study, two-thirds of the participants who took the Cologuard test showed false-positive results. A positive test result from the stool or blood test requires a colonoscopy to validate the results. And because the blood or stool test is considered the “screening” test, the follow-up colonoscopy is regarded as the “diagnostic” colonoscopy. A colonoscopy serves to detect and prevent cancer as it identifies over 95% of dangerous, precancerous polyps and removes them at the procedure time. It can also enable the capture of tissue samples for pathology testing to determine more accurately if cancerous cells are present. As a result, the colonoscopies are far more conclusive and provide preventative measures by removing any polyps identified in the colon. This procedure is a “screening” colonoscopy. Suppose any polyp/tissue is identified and removed during the screening colonoscopy, and pathology markers do not indicate the presence of any pre-cancerous or cancer. In that case, another screening colonoscopy is typically not required for ten (10) years.
There are three primary categories for the use of a colonoscopy:
Screening/Preventative Colonoscopy – is conducted typically for asymptomatic individuals (no gastrointestinal symptoms either past or present) who at age 45+ are establishing a baseline screening to ensure they are not at early risk for colon cancer. A Screening colonoscopy enables the physician to look for any abnormality in the colon, be it polyps, abnormal cells, and the like. At the time of a screening colonoscopy, polyps, which can turn into cancerous cells, can be removed, and tissue samples obtained to determine if cancerous cells are present in the colon. A screening colonoscopy is recommended once every ten (10) years for asymptomatic patients aged 45-75 with no personal or family history of colon polyps, gastrointestinal disease, or colon cancer. Most insurance carriers typically cover screening colonoscopies as a preventative measure. It is essential to check with the insurance provider before having any procedure to know what is covered and any expected out-of-pocket costs associated with this procedure under the individual patient’s policy.
Surveillance Colonoscopy – is conducted when a patient has a personal history of colon polyps, gastrointestinal disease, or cancer but may be asymptomatic (no gastrointestinal symptoms either past or present). The need for a surveillance colonoscopy can vary based on the patient’s personal history. Note that patients with a history of colon polyps would receive a surveillance colonoscopy and likely undergo additional surveillance procedures at shortened intervals (e.g., every 2-5 years). It is essential to check with the insurance provider before having any procedure to know what is covered and any expected out-of-pocket costs associated with this procedure under the individual patient’s policy.
Diagnostic/Follow-up Colonoscopy is when a patient presents with or has a history of gastrointestinal symptoms, polyps, anemias, or a gastrointestinal disease/diagnosis. The patient’s history and findings from any previous colonoscopy determine the need for a follow-up/diagnostic colonoscopy. For example, if a patient conducts a non-invasive screening for colorectal cancer, such as FIT or Cologuard, and receives a positive result of any kind, a diagnostic/follow-up colonoscopy would be required to validate the findings of the initial screening test. Diagnostic colonoscopies often result in out-of-pocket payments. Therefore, it is essential to check with the insurance provider before having any procedure to know what is covered and any expected out-of-pocket costs associated with this procedure under the individual patient’s policy. Bottom line, if you are 45 years of age or older, you need to have a colorectal cancer screening as a baseline and preventative measure for long-term colon health. It is crucial to understand the differences between available colon cancer screenings and what to expect with each. And, colonoscopy remains the most effective form of cancer detection and the ONLY form of colon cancer prevention available. If you have more questions about home screenings or want to schedule a colonoscopy, reach out to one of the GI Alliance doctors in your area to discuss your options. Colon cancer screening saves lives. Your life is worth a simple, painless procedure to help ensure your long-term health.
Find a GI Alliance physician near you at www.gialliance.com/locations/.
Sources: U.S. Preventive Services Task Force.
Final Recommendation Statement, Colorectal Cancer: Screening. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening American Society for Gastrointestinal Endoscopy. https://ww-w.asge.org/home/about-asge/newsroom/media-backgrounders-detail/colorectal-cancer-screening Society Task Force on Colorectal Cancer. The American Journal of Gastroenterology 2017;112:1016-1030. http://doi.org/10.1038/ajg.2017.174 U.S. Food and Drug Administration. Summary of Safety and Effectiveness Data (SSED). https://www.accessdata.fda.gov/cdrh_docs/pdf13/P130017b.pdf Gastrointestinal Endoscopy Journal, Volume 93, No. 6S: 2021 AB95


