The First Brain and the Second Brain (Part 2)
9/24/2019
The amazing human body has two brains: the one we are all familiar with that is encased in the skull and a lesser-known but equally important one found in the human gut. The connection between the two brains is so close, when one gets upset, the other does too. In Part 1, we talked about how the two brains are connected. In Part 2, we’re talking about how to measure the fitness level of your brain and how to strengthen your brain with customized brain fitness exercises. If you missed Part 1, read it here.
When patients visit the office of their medical doctors, standard tests and procedures are performed to allow for appropriate diagnostic and optimal intervention recommendations.
At the medical practice of Dr. Mona Dave, a patient may have tests done upon the initial visit, such as upper and lower endoscopy. Based on the results of the tests performed, the patient is then provided an overview of results and recommendations to best treat their condition or concern.
Brain Fitness can now similarly be measured by gold standard tests, which then allow an experienced provider to ascertain best possible interventions and training programs.
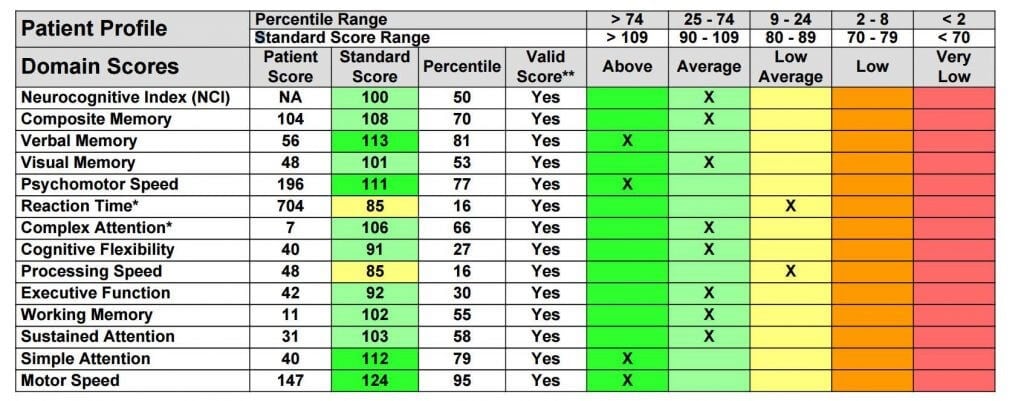
In Part 1 of this two-part blog, I mentioned one of Dr. Dave’s patients whose medical tests were in the clear, thereby prompting a referral to look at brain fitness levels as being possible contributors to gut concerns. The NeuroCognitive assessments will show distinct patterns of the brain, potentially revealing a brain that is primarily wired for anxiety (which has numerous gut interactions), or a brain that has the wiring of poor sleep and attention concerns, or perhaps one with a history of concussion/traumatic brain injury.
All of these patterns can be specifically measured, with detailed reports outlining severity and specific location in the brain where the level of performance is under or overactive.
![neurocognitive assessment]() The second assessment to measure the electrical activity of the brain is a Quantitative Electroencephalograph (QEEG), often referred to as a “brain map.” The report provided is 60 pages and includes analysis of Traumatic Brain Injury and Learning Disability.
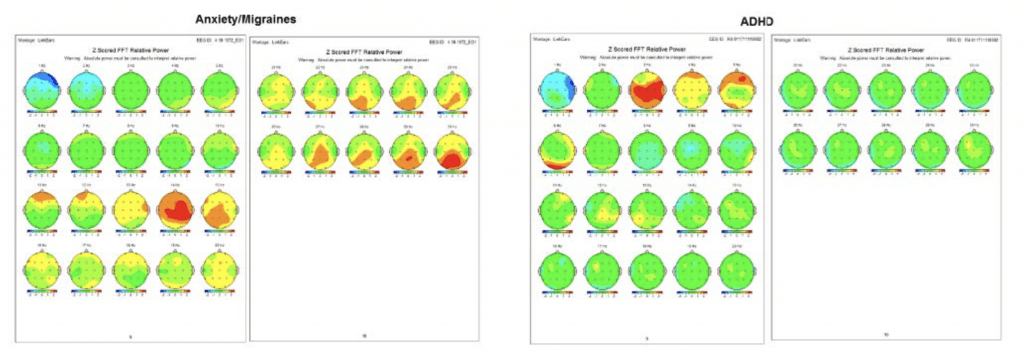
Examples of some patterns we can see in the full Quantitative Electroencephalograph Assessment:
The second assessment to measure the electrical activity of the brain is a Quantitative Electroencephalograph (QEEG), often referred to as a “brain map.” The report provided is 60 pages and includes analysis of Traumatic Brain Injury and Learning Disability.
Examples of some patterns we can see in the full Quantitative Electroencephalograph Assessment:
![First Brain Pt. 2_2]() Put very simply, green is “good”; areas showing yellow, orange, or red are “too much of that brain wave in that part of the brain”; and areas showing blue are “not enough of that brain wave in that part of the brain.”
Put very simply, green is “good”; areas showing yellow, orange, or red are “too much of that brain wave in that part of the brain”; and areas showing blue are “not enough of that brain wave in that part of the brain.”
![quantitative electroencephalograph assessment]()
![First Brain Pt. 2_5]() Then what? Once have comprehensive brain fitness assessments, customized training program can be tailored.
Then what? Once have comprehensive brain fitness assessments, customized training program can be tailored.
![]() For a complimentary consultation on how to have your brains fitness assessed and learn ways to optimize your brains fitness, contact NeuroCognitive Fitness LLC.
Dee O’Neill-Warren is a licensed professional counselor, board certified in Neurofeedback. She sees clients via private practice at 4101 McEwen Drive, Suite 670, Dallas, Texas, or via concierge mobile service. For more information, check out website www.neurofitnow.com, call 972-638-7689, or email [email protected].
If you would like more information about gastrointestinal (GI) digestive disorders and nutrition in children, please contact Dr. Mona Dave’s Plano Office or Southlake Office.
For a complimentary consultation on how to have your brains fitness assessed and learn ways to optimize your brains fitness, contact NeuroCognitive Fitness LLC.
Dee O’Neill-Warren is a licensed professional counselor, board certified in Neurofeedback. She sees clients via private practice at 4101 McEwen Drive, Suite 670, Dallas, Texas, or via concierge mobile service. For more information, check out website www.neurofitnow.com, call 972-638-7689, or email [email protected].
If you would like more information about gastrointestinal (GI) digestive disorders and nutrition in children, please contact Dr. Mona Dave’s Plano Office or Southlake Office.
How to Measure Brain Fitness with NeuroCognitive Assessment:
MEASURE:- Computerized Cognitive Assessment & self-report questionnaires via Central Nervous System Vital Signs (CNS-VS)
- Brain map, Quantitative Electroencephalograph (QEEG)
 The second assessment to measure the electrical activity of the brain is a Quantitative Electroencephalograph (QEEG), often referred to as a “brain map.” The report provided is 60 pages and includes analysis of Traumatic Brain Injury and Learning Disability.
Examples of some patterns we can see in the full Quantitative Electroencephalograph Assessment:
The second assessment to measure the electrical activity of the brain is a Quantitative Electroencephalograph (QEEG), often referred to as a “brain map.” The report provided is 60 pages and includes analysis of Traumatic Brain Injury and Learning Disability.
Examples of some patterns we can see in the full Quantitative Electroencephalograph Assessment:
 Put very simply, green is “good”; areas showing yellow, orange, or red are “too much of that brain wave in that part of the brain”; and areas showing blue are “not enough of that brain wave in that part of the brain.”
Put very simply, green is “good”; areas showing yellow, orange, or red are “too much of that brain wave in that part of the brain”; and areas showing blue are “not enough of that brain wave in that part of the brain.”
Stroke
Example of client with recent stroke. The back left part of brain shows overly powerful slow wave patterns (yellow, orange, and red) in Delta and Theta wavelengths of EEG, as well as underactive patterns of Beta wavelengths, our thinking brain speed. Then what? Once have comprehensive brain fitness assessments, customized training program can be tailored.
Then what? Once have comprehensive brain fitness assessments, customized training program can be tailored.
A National Call for Action: From the Kennedy Forum Report; Brain Health and Brain Fitness
“Brain Fitness is the Key: Neuroscience shows that brain fitness interventions can build higher-order processing skills, promote emotional resilience, and mitigate stress.” Sample of Key Interventions listed in Kennedy Forum Report:- Neurofeedback – Provides self-reflective feedback loops that allow individuals to witness brain activity and increase and improve Executive Function skills, such as attention, focus, and other cognitive abilities.
- Executive Function Training – Increases and improves higher-order processing, engages the prefrontal cortex (PFC) in learning and decision-making
- Mindfulness Training – Allows for purposeful brain regulation that increases and improves ability to be present, maintain attention, down-regulate disruptive emotions, and direct learning and social input to higher-order processing.
NeuroCognitive Training Options
Customized training programs determined from assessments above and clinical interview.- Neurofeedback Training to manage stress and build resilience.
- Cogmed Working Memory Training program to increase working memory capacity, necessary for staying focused on a task, blocking out distractions, and keep you updated and aware of what’s going on around you.
- Alpha-Stim Cranial Electrotherapy Simulation (CES) to quickly and safely relieve symptoms of anxiety, depression, and insomnia.
 For a complimentary consultation on how to have your brains fitness assessed and learn ways to optimize your brains fitness, contact NeuroCognitive Fitness LLC.
Dee O’Neill-Warren is a licensed professional counselor, board certified in Neurofeedback. She sees clients via private practice at 4101 McEwen Drive, Suite 670, Dallas, Texas, or via concierge mobile service. For more information, check out website www.neurofitnow.com, call 972-638-7689, or email [email protected].
If you would like more information about gastrointestinal (GI) digestive disorders and nutrition in children, please contact Dr. Mona Dave’s Plano Office or Southlake Office.
For a complimentary consultation on how to have your brains fitness assessed and learn ways to optimize your brains fitness, contact NeuroCognitive Fitness LLC.
Dee O’Neill-Warren is a licensed professional counselor, board certified in Neurofeedback. She sees clients via private practice at 4101 McEwen Drive, Suite 670, Dallas, Texas, or via concierge mobile service. For more information, check out website www.neurofitnow.com, call 972-638-7689, or email [email protected].
If you would like more information about gastrointestinal (GI) digestive disorders and nutrition in children, please contact Dr. Mona Dave’s Plano Office or Southlake Office.